HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 7 days back then he developed fever which is insidious in onset , gradually progressive , high grade fever , increased during night , associated with chills and rigors , no aggravating factors , relieved temporarily on medication
History of night sweats
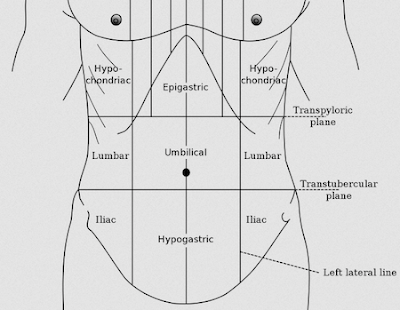
Then he developed pain abdomen since 1 week which was insidious in onset , gradually progressive , pain in right hypochondrium , right lumbar , umbilical region which was pricking type , non radiating , aggrevated on inspiration , non relieving factor
H/o cough since 3 days insidious on onset , non productive
No h/o post nasal drip , sore throat , running nose , nasal congestion , headache
No h/o constipation , nausea , vomiting , loose stools , abdominal distension
No h/o dypsnea , wheezing
No h/o chest pain , palpitations , pnd,orthopnea , platypnea
No h/o hemoptysis , hoarseness of voice , burning micturition
PAST HISTORY
10 days back had an episode of fever which subsided on medication H/o of hospital admission in hospital 9 days back , where he was non relieved and came to our hospital
Not a k/c/o hypertension , diabetes , asthma , epilepsy , tuberculosis
PERSONAL HISTORY
Diet - mixed
Sleep - disturbed
Appetite - normal
Bowel and bladder movements - regular
Addictions - ocassionally drinks alcohol
No smoking habits
No allergies
FAMILY HISTORY
No significant family history
TREATMENT HISTORY
Pleural tap done on 14.04.23 ( 20 ml ) and on 15.04.23 (30 ml )
GENERAL EXAMINATION
Patient was conscious , coherent , cooperative
Moderately built , moderately nourished
No signs of pallor
Icterus - absent
Cyanosis - absent
Clubbing - absent
Kolionychia - absent
Lymphadenopathy - absent
Edema - absent
Vitals
Pulse - 86
Bp - 120/ 80 mmhg
Temp - afebrile
Rr - 16 cpm
RESPIRATORY SYSTEM
INSPECTION
Trachea appears to Be midline
Chest movements appears to Be equal
Shape of chest appears to Be elliptical
No scars , no sinuses , engorged veins
No hallowing , no crowding of ribs , drooping of shoulder
PALPATION
All inspectory findings are confirmed
No Local rise of temperature
No tenderness
Trachea - central
Bilateral chest movements are equal
No palpable swelling , masses
Vocal fremitus - Rt. Lt
Supraclavicular : N N
Infraclavicular : N. N
Mammary : Decreased N
Inframammary : decreased. N
Axillary : Decreased. N
Infraaxillary : decreased. N
Suprascapular : N. N
Infrascapular : N. N
Interscapular : N. N
PERCUSSION - Rt. Lt
Supraclavicular : R R
Infraclavicular : R R
Mammary : Decreased R
Inframammary : decreased R
Axillary : Decreased R
Infraaxillary : decreased R
Suprascapular : R R
Infrascapular : R R
Interscapular : R R
Auscultation - Rt Lt
Supraclavicular : NVBS NVBS
Infraclavicular : NVBS NVBS
Mammary : Ab NVBS
Inframammary : Ab NVBS
Axillary : NVBS NVBS
Infraaxillary : NVBS NVBS
Suprascapular : NVBS NVBS
Infrascapular : NVBS NVBS
Interscapular : NVBS NVBS
PER ABDOMEN
INSPECTION
Shape of abdomen - appears to Be scaphoid
Umbilicus - appears to Be inverted
No scars , no swellings , engorged veins
No visible pulsations , no peristalsis
PALPATION
Local rise of temperature is seen
Tenderness in right hypochondrium , right lumbar , umbilical region
No mass felt
PERCUSSION
No h/o fluid thrill , liver span , shifting dullness
AUSCULATION
Bowel sounds are heard
CVS
No chest wall abnormalities
No scars sinuses sinuses engorged veins
Trachea appears to be central
Apical impulse not visible
PALPATION
Apical impulse felt at 5th ics 1cm medial to midclavicular line
No parasternal heaves
No thrills
Auscultation
S1 s2 heard no murmurs
CNS
Higher mental functions :intact ,normal
Cranial nerves :normal
Sensory examination: Normal sensations felt in all dermatomes
Motor examination: normal tone,power in upper and lower limbs, normal gait
Reflexes: B/l elicited
Cerebella’s function: normal
No meningeal signs were elicited
INVESTIGATIONS
FEVER CHART :
USG REPORT
PROVISIONAL DIAGNOSIS
Right sided Pleural effusion secondary to TB with mild hepatospleenomegaly.
Iv fluids NS
Inj neomol 1gm iv
Inj tramadol 1amp in 100 ml of NS
Inj pan 40mg
T.azithromycin 500mg
Tab ATT
4 tabs H 340mg,R 680mg,Z 1700mg,E 1020mg
Tab PCM 650mg
Syrup grilintus 15ml
Tab pyridoxine 25mg
Inj diclofenac I.m










Comments
Post a Comment