My experiences with general cellular and neural cellular pathology in a case based blended learning ecosystems
आरोग्यम् परमं भाग्यं स्वास्थ्य
्यं सर्वार्थ साधनम्।
शरीरं सुखमायान्ति सततं
Translation:
“ Good health is the greatest blessing, and well-being is the means to achieve all goals.
In a body where health is constant, happiness always prevails. “
ज्ञानं परं बलं तपः।
ज्ञानेन विनयो यत्र।
ज्ञानाद्धर्मो यशः सुखं।
ज्ञानेन विना न जीवनं॥
Translation:
" Knowledge is the supreme power, the source of self-discipline.
Where there is knowledge, there is humility.
Through knowledge, one attains righteousness, fame, and happiness.
Without knowledge, life is meaningless."
In my belief, Since the inception of philosophy and medical science, knowledge and health combined together uphold the prosperity of the human race. Moreover, it helps humans in sustaining the thing that’s most precious to them, life.
Greetings. I am Anurag Vaddadi, a medical student currently in final year of MBBS and welcome to my memoir of clinical experiences regarding Clinical based blended learning and blogging through PaJR. The need for continuous clinical knowledge and exposure can never be met, as a clinician is always learning till his last breath. A subject that is never saturated, always intriguing. Oh, why don’t we just go ahead and call it a boon that never stops giving?
Life is nothing without ambition and innovation.
I express my deepest gratitude to my college and professors for letting me be a part of this esteemed learning ecosystem that has motivated me to learn and grow as a clinician and an individual.
During my clinical posting in November, I came across a rather common case wherein a 55 year old farmer from Nalgonda presented with a multitude of complaints that required a thorough history taking and careful clinical examination to arrive at a conclusive diagnosis.
This being the first case that I was taking in final year, the need for thorough examination and exhaustive history taking was apparent to me more than ever, especially since practical experience and knowledge weigh more in a world dominated by the power of theory.
The patient expressed chief complaints of abdominal pain, which he had been experiencing for the past four months. This was accompanied by abdominal bloating and persistent belching, suggestive of underlying gastrointestinal issues. However, the presence of additional symptoms raised my suspicion about a potential systemic problem.Upon further inquiry, the patient revealed that he had been experiencing shortness of breath on exertion and palpitations for the past month.
Learning point : These symptoms pointed towards a possible cardiovascular component, prompting us to investigate whether there was an interplay between his abdominal complaints and his cardiac function.
I then further moved forward by conducting a detailed medical history, paying particular attention to any significant changes in his lifestyle, diet, or medication regimen. We also assessed his family history, looking for any genetic predisposition to certain conditions but didn’t find any.Subsequently, a series of investigations were ordered. Blood tests were conducted to evaluate his hemoglobin levels, which revealed a significant decline, thus prompting a closer examination of his blood profile. A complete blood picture (CBP) and peripheral smear were performed, which demonstrated microcytic and hypochromic red blood cells, indicating iron deficiency anemia.The discovery of iron deficiency anemia shed light on the underlying cause of the patient's symptoms. It became evident that the anemia was responsible for his fatigue, shortness of breath on exertion, and palpitations. However, the challenge remained in determining the cause of his iron deficiency.To gain further insight, we delved into the patient's medical records and conducted additional investigations. We explored potential sources of chronic blood loss, such as gastrointestinal bleeding, which could lead to iron deficiency anemia. Further tests, including upper gastrointestinal endoscopy and colonoscopy, were scheduled to evaluate the integrity of his gastrointestinal tract and identify any possible bleeding sources.Throughout the patient's evaluation and treatment, I worked closely with the attending physician to develop a comprehensive management plan. We addressed the patient's iron deficiency through a combination of oral iron supplements and dietary modifications, emphasising the importance of incorporating iron-rich foods into his meals with his wife through interactive case history taking.
Learning point :
Holistic Patient Assessment -- conducting a thorough physical examination, taking into account vital signs, general appearance, and specific system examinations. This approach allowed for a comprehensive evaluation of the patient’s overall health and identification of any additional findings.
This case not only highlighted the complexity of diagnosing and managing patients with multiple presenting complaints but also highlighted the importance of a systematic and interdisciplinary approach. It reinforced the significance of thorough history-taking, diligent examination, and judicious utilisation of diagnostic tools in order to unravel the underlying etiology and provide appropriate management.
This is me, witnessing this patient's journey from presenting with a cluster of seemingly unrelated symptoms to being diagnosed with iron deficiency anemia. It proved to be an invaluable learning experience for me.
https://anuragvaddadi.blogspot.com/2022/12/55-year-old-with-abdominal-pain.html
A day prior to our Pre-final examination, we were required to take up a case when I had the chance to see an interesting one involving a 35-year-old male patient who presented to the clinic with severe pain in the right hypochondrium for the past five days. The following is a narration of my experience in evaluating and managing this patient.
Upon taking the patient's history of presenting illness, it was revealed that he had been asymptomatic until five days ago when he suddenly developed severe pain in the right flank. The pain was not radiating and was associated with fever, which had improved after taking medication two days before. The patient also reported experiencing weakness and headache four days ago. Additionally, he had developed a dry cough four days ago, not associated with sputum production. Furthermore, he complained of intermittent burning chest pain due to indigestion and acid reflux, aggravated by eating oily food which the patient admitted to consuming everyday.
I also wondered if the pain, weakness, fever and headache were interrelated, suggesting an inflammation in the right hypochondrium?
As part of the personal history assessment, the patient reported a decreased appetite since the onset of pain. His diet was mixed, and he had been experiencing disturbed sleep due to the pain, waking up on an average 2 times per night. His bowel and bladder movements had decreased. He had a history of alcohol intake, consuming 90ml daily, but denied any history of smoking. There was no history of similar complaints in his family. Upon conducting a general examination, even though the patient was conscious, coherent and cooperative, he had a bad temper and was uncomfortable by the presence of us students around him. He had a moderate build and moderate nourishment. Systemic examination of Cardiovascular system, respiratory system were normal.
The importance of examination findings and perfecting them was what got me pretty rumbled at first, then with the help of my peers and our helpful Post graduate seniors, I was motivated into a web of constant learning through more and more examination attempts on this patient and the ones on other beds too.Considering the patient's clinical presentation and examination findings, along with the provisional diagnosis, we decided to proceed with further investigations, including an ultrasound (USG). The USG would provide more insight into the suspected liver abscess, grade I fatty liver, and cholelithiasis.
Based on the provisional diagnosis of liver abscess with grade I fatty liver and cholelithiasis, the management plan was formulated. Treatment was initiated with Intravenous Piperacillin-Tazobactam, Intravenous Metronidazole, Intravenous Fluids - Normal Saline and Ringer's Lactate over a 100 ml/hr IV infusion, Intravenous Optineuron – a neurotropic vitamin, and Inj. Zofer.
Learning points :
I appreciated the importance of thorough history taking for accurate diagnosis and management.
Association of multiple symptoms was necessary in determining the diagnosis.
I had also found out the importance of considering lifestyle factors and personal history in the overall assessment and management of the patient.
As this blog was made for my Pre-final examination, the following questions were asked by the Senior residents:
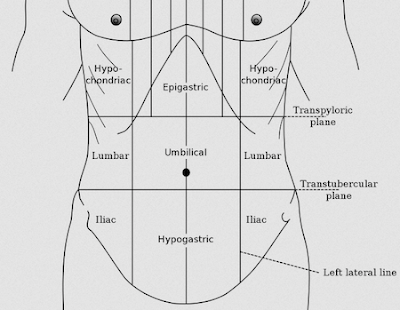
1. Name the quadrants of the abdomen?
2. What is double target sign? The double target sign is a characteristic radiological finding of liver abscess described in contrast enhanced CT images. The appearance is generated by 2 concentric rings of various attenuations surrounding a central hypodense fluid filled area giving a stratified pattern to the hepatic lesion which resembles a target.The low attenuation central zone represents liquified necrotic tissue. The higher attenuation in a rim represents the pyogenic membrane. While the low attenuation outer layer is due to the localised zone of edema of the liver parenchyma.
Source : https://www.researchgate.net/publication/323556188_The_double_target_sign_in_liver_abscess
3. Differential diagnosis of pyogenic liver abscess?
Hydatid cyst
Cholecystitis
Hepatocellular carcinoma
Biliary disease
Their questions made me delve further into the etiology of the disease, thus enabling me to better understand the case better, which moving forward I can use to my advantage in the clinical setting. https://anuragvaddadi.blogspot.com/2022/12/35-year-old-male-with-pain-in-right.html
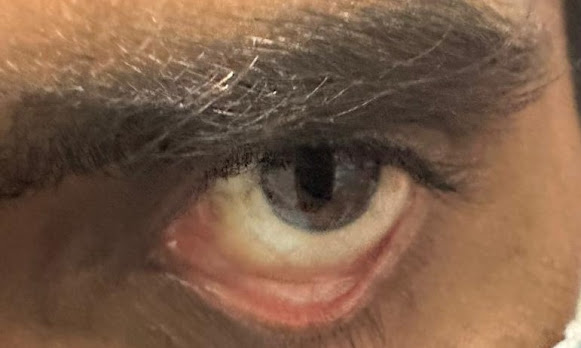
On another day of my clinical posting, I had the opportunity to see a fascinating case involving a 55-year-old male shopkeeper who presented to the hospital with complaints of lower back pain for the past five years and chest pain for the past two years. This patient's medical history and current symptoms provided valuable insights into the importance of clinical learning on both a logical and emotional level.Taking the history of presenting illness revealed that 23 years ago, the patient experienced symptoms of polydipsia, polyuria, and polyphagia, which led to a diagnosis of Type 2 Diabetes Mellitus. Since then, the patient has been on antidiabetic medication. He currently experiences occasional episodes of tingling sensation and blurred vision, which could be attributed to diabetic neuropathy. Ten years ago, the patient had an episode of hematuria and was diagnosed with High-Grade Urothelial Bladder Carcinoma without muscular involvement. Surgical excision of the growth and subsequent treatment with BCG installation were undertaken. The patient has been advised regular follow-ups every two years since then.Seven years ago, he was diagnosed with hypertension, for which the patient has been taking Olmesartan Medoxomil 40 mg. Additionally, five years ago, the patient fell from a terrace, when he experienced subsequent lower back pain. The pain was dull in character, radiating to the front, and worsened with prolonged sitting but was relieved upon changing position or stretching. The treatment history revealed that there was a surgical excision of the bladder carcinoma growth, followed by BCG instillation as a part of medical management. The patient's current medication includes Metformin Hydrochloride, Glimepiride, Vildagliptin, and Olmesartan Medoxomil. Regarding personal history, the patient's appetite was reported as normal, with a mixed diet and adequate sleep. Bowel and bladder movements were normal, and there were no reported allergies. However, the patient did have a history of chronic smoking, consuming 2-4 cigarettes a day, while alcohol consumption was absent. The patient's grandfather had a history of Type 2 Diabetes Mellitus, but there was no family history of cancer. During the general examination, the patient appeared conscious, coherent, and well-oriented. Various investigations were ordered as part of the patient’s evaluation, including an ultrasound, ECG, and X-ray of the abdomen. Biochemical investigations were also planned to obtain a comprehensive understanding of the patient's condition.
Based on the available information, the provisional diagnosis was Type 2 Diabetes Mellitus with a history of carcinoma of the urinary bladder. The treatment plan involved prescribing Tablet Gemer 2mg and Tablet Vylda-M 50/500 to manage diabetes and its associated symptoms.
Learning point :
- Significance of lifestyle assessment : paying attention to the patient’s personal history, particularly appetite, diet, sleep, bowel and bladder movements, and addictions. Recognising the impact of lifestyle factors on overall health and disease management is important for providing comprehensive care to patients.
- Emotional Impact of Clinical Encounters : importance of empathetic and compassionate interaction in addition to clinical knowledge and skills.
Reflecting on this case, it threw light on the importance of clinical learning on a logical and emotional level. The patient's complex medical history, including diabetes being a rampant ever existing disease and it’s effects on the overall holistic health of the patient made me spiral down into a web of introspection, while I questioned my own lifestyle choices and decisions. https://anuragvaddadi.blogspot.com/2022/12/56-year-old-male-with-type-2-diabeties.html
As a medical student, I encountered a case that roused my interest. An 85-year-old male patient presented to the hospital with the following chief complaints: Fever since 3 days, 2 episodes of involuntary movements of the upper limb and lower limb in the past 3 days, Loose stools since 1 day. The patient's history of present illness (HOPI) revealed that he was asymptomatic three days prior to his visit when he developed a high-grade fever accompanied by chills. Subsequently, he experienced two episodes of seizures, characterised by involuntary movements of the upper and lower limbs. During these episodes, the patient also had involuntary micturition and passage of stools. Seeking medical attention, he consulted a local RMP (Registered Medical Practitioner) who prescribed some medications and sent him home. On the following day, the patient had a similar seizure episode. Concerned, he decided to come to the hospital on the third day of his illness. Additionally, he reported the passage of loose stools, which were not blood-tinged, foul-smelling, or sticky. Regarding the patient's past medical history, extensive history taking was attempted in terms of personal history, but the patient allowed limited interaction, showing disinterest in our interactive history taking methods. He claimed to have had no addictions and also complained of difficulty in holding urine, and had regular sleep patterns.Upon conducting a general examination, I found the patient to be conscious and coherent. Systemic examination of the cardiovascular system revealed normal heart sounds (S1 and S2) without any additional sounds. Chest expansion was equal on both sides. Percussion and auscultation yielded normal findings. Abdominal examination indicated a soft abdomen, non-tender, without ascites.The central nervous system (CNS) examination revealed intact higher mental functions and normal cranial nerve responses. On assessing the motor system, there were no abnormalities observed in muscle bulk, tone, or power. Reflexes were intact and symmetrical. The sensory system showed normal findings. Further investigations, including an MRI of the brain, ultrasound, 2D echocardiography, and chest X-ray, were conducted to gather more information and aid in the diagnosis. Based on the patient's clinical presentation and investigations, the provisional diagnosis was determined as febrile delirium (with two episodes of generalised tonic-clonic seizures), dengue NS1 positive with thrombocytopenia, and the absence of diabetes and hypertension. Treatment for the patient included intravenous fluids (normal saline and Ringer's lactate) at a rate of 75 ml/hr and the administration of Levipill 500 mg orally twice daily.Questions
1. What are the potential risks and benefits of initiating anti-seizure medication in an elderly patient with febrile delirium?
Ans: Clearly the data on antiepileptic drugs in the elderly are scarce. With enough clinical experience of use of older antiepileptics in the general population, phenytoin, carbamazepine and valproate are still the choice of drugs in elderly. Newer AEDs have shown relatively fewer interactions and lesser adverse effects while providing equivalent seizure protection. “Start low and go slow” technique should be followed in the elderly. Source : https://link.springer.com/article/10.1007/s13760-019-01132-4 (Antiepileptic drug therapy in the elderly: a clinical pharmacological review) 2. How would you differentiate between febrile delirium and other conditions presenting with similar symptoms? Ans: The clinical history, physical examination, and laboratory studies are helpful in distinguishing delirium from other causes of global cognitive impairment, such as dementia, depression, and functional psychosis. Dementia has a gradual onset, persists for more than 1 month, is usually progressive, and is not associated with reduced alertness until a terminal stage. Dementia, however, predisposes to delirium, and the sudden deterioration of cognitive or functional ability in a demented patient. Source : https://www.sciencedirect.com/science/article/abs/pii/S0025619611643802 3. What are the possible complications associated with dengue fever and thrombocytopenia in this case? Ans: Possible complications are haemorrhage, organ dysfunction, and fluid imbalances. Close monitoring of platelet counts, fluid balance, and vital signs is crucial to detect and manage any potential complications. Throughout this case, I was faced with various challenges and questions that needed to be addressed. By consulting with experienced postgraduates for help, discussing the case in clinical rounds, and conducting further research, I was able to enhance my understanding of the patient's condition and improve my clinical approach towards the patient and articulate the logic and reasoning behind the everlasting pair of Textbook and clinical knowledge. I feel, clinical experiences like this play a vital role in a medical student's education, enabling us to apply theoretical knowledge to real-life scenarios and develop critical thinking skills necessary for future medical practice. https://anuragvaddadi.blogspot.com/2022/12/85-yr-old-male-with-seizures-following.html


Comments
Post a Comment