This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis "to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
December 6th 2022
Anurag K Vaddadi
Roll no: 189
Case
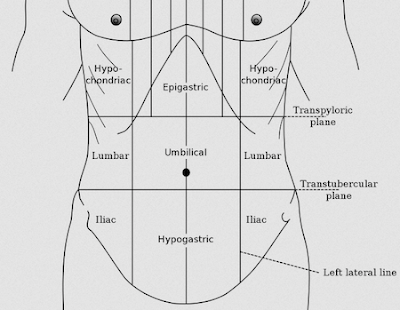
A 35 year old male patient came with chief complaints of pain in the right hypochondrium since 5 days.
History of presenting illness:
Patient was apparently asymptomatic 5 days back, then he developed pain in the right hypochondriac region which was sudden in onset, non-progressive. Pain is severe and non-radiating type and is associated with fever which was relieved on taking medication 2 days back. It was associated with weakness 4 days ago, along with headache.
Simultaeneously he developed dry cough 4 days ago, not associated with sputum.
Patient also experienced burning type of chest pain due to indigestion and acid reflux, intermittent in nature, aggravated by intake of oily food.
No history of nausea, vomiting, weight loss or shortness of breath.
History of past illness
No similar history in the past.
History of ulcer 10 years ago, treated with proton pump inhibitor (omeprazole)
No History of Hypertension/Diabetes Mellitus/ Asthma/CAD/ epilepsy
Personal History
Appetite : decreased since 5 days
Diet : mixed
Sleep : disturbed sleep due to pain
Bowel &
bladder movements : Decreased
Addictions : History of alcohol intake, 90ml everyday,
No history of smoking
Family History
No similar complaints in the family.
General examination:
Done after taking consent. Patient is conscious, coherent and cooperative, well oriented to time, place, person. Moderately built and moderately nourished.
VITALS
Temperature 97 F
BP 130/80 mmHg
PR 88/ min
RR 20/min
SpO2 97 %
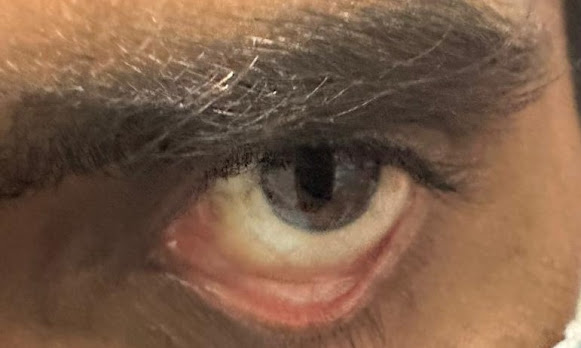
Mild Icterus present
No pallor, cyanosis, clubbing or generalised oedema or lymphadenopathy
SYSTEMIC EXAMINATION
CVS
S1,S2 sounds heard
RESPIRATORY SYSTEM
BAE +
Normal Vesicular Breath Sounds
P/A : On inspection: abdomen symmetrical with no visible pulsations or scars.
On palpation: soft, pain Elicited in right hypochondrium.
Liver not palpable
On Auscultation: Bowel Sounds - Heard
CNS : No focal neurological defect.
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Liver Abscess with Grade I Fatty Liver and cholelithiasis.
MANAGEMENT :
1.Inj. PIPTAZ 4.5g/ IV/ TID
2. Inj. METROGYL 500 mg/IV/ TID
3. IVF - NS and RL : 100 ml/hr IV infusion
4.Inj. OPTINEURON 1 Amp in 100 ml NS/ IV/ over 30 mins
5. Inj. Zofer 4mg/ IV/s.o.s


.jpeg)

Comments
Post a Comment