55 year old with abdominal pain.
Date: November 20th 2022
This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis "to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
November 20th 2022
Anurag K Vaddadi
Roll no: 189
Case
A 55 year old patient came with chief complaints of:
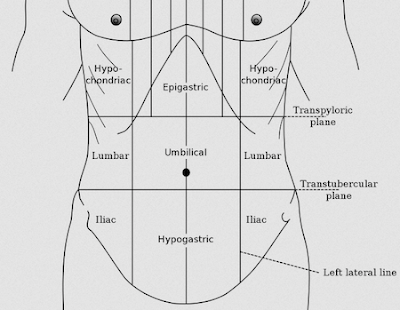
1) Abdominal pain since 4 months
2) Abdominal bloating since 4 months
3) Belching since 4 months
4) Shortness of breath on exertion since 1 month
5) Palpitations since 1 month
VITALS
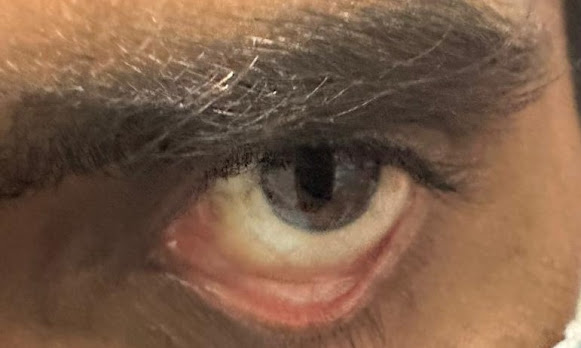
Pallor present
CVS
RESPIRATORY SYSTEM
- peripheral smear
- blood grouping and typing
- blood urea
- serum creatinine
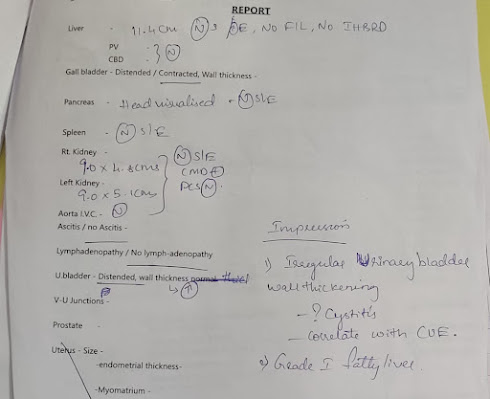
- usg
2. TAB. OROFER - XT
3. TAB. RANTAC
4. INJ. Ferric carboxymaltose 500 mg/ iv
.jpeg)


.jpeg)


.jpeg)

Comments
Post a Comment