This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis "to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
A 57 year old female, agricultural labourer by occupation, resident of neernemula, came to the casualty with the chief compliants of:
Fever since 10 days
Burning micturition since 8-9 days
Decreased appetite and generalised weakness since 4 days
vomitings since 2days
HOPI:
Patent was apparently asymptomatic 10 days ago then she developed fever intermittent type, associated with chills, which was followed by burning micturition from the next day.
She had 2 episodes of vomitings (Last night and today morning) which is Non bilous, non projectle with water as it's contents.
H/O Decreased appetite since 4 days
Generalised weakness since 4 days
H/O regurgitation of food +
Retrosternal burning sensation +
No H/O abdominal pain, loose stools & constipation
No H/o hematuria, frothy urine.
No H/o loss of weight
PAST HISTORY
Not a K/C/O DM/HTN/TB/Asthma/CAD/Epilepsy.
PERSONAL HISTORY
Appetite: decreased since 4days
Diet: mixed
Bowel habits: regular, bladder: burning micturition since 8-9 days
Sleep: adequate
Addictions: Nil
FAMILY HISTORY
No significant family history
GENERAL EXAMINATION:
Patient is conscious, cohorent, cooperative.
Pallor- absent
Icterus- absent
Clubbing-absent
Lymphadenopathy- absent
Cyanosis- absent
Pedal edema - absent
VITALS at presentation:
Pt is febrile on touch, Temp: 101.9 F
B.P: 130/100 mmhg
P.R: 110bpm
R.R: 16 cpm
SPO2: 98% on RA
GRBS: 112 mg/dl
SYSTEMIC EXAMINATION:
CVS - S1, S2 heard no murmurs
RS - bilateral air entry present
Normal vesicular breath sounds heard in all areas
PER ABDOMEN - soft
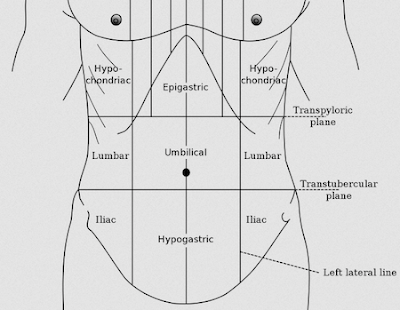
Mild tenderness noted in right hypochondriac and epigastric region.
CNS - HMF intact, No focal neurological deficits
CHEST X-RAY
X-RAY OF HAND:
LAB REPORTS:





















Comments
Post a Comment