This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis "to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
A 61 year old male patient came to the hospital with chief complaints of :
CHIEF COMPLAINTS
Dry cough since 10 days
Dragging pain towards the finger tips since 10 days
Lower back pain since 10 days
Shortness of breath
Chest pain near heart since 10 days
HISTORY OF PRESENTING ILLNESS
PATIENT WAS APPARENTLY ASYMPTOMATIC 3 YEARS AGO WHEN
He noticed involuntary movements of upper right limb at rest and decreased on movement
2 years ago he increased the intake of alcohol, then 1 year back he noticed slowing of movements and decrease in his pitch of voice.
He has used medication but stopped after 5 months due to lack of improvement of symptoms,
Since 20 days back he has trouble recollecting and takes at least 30-40 minutes to perform any activity.
10 days back he experienced dry cough,
Lower back pain on both sides draging type radiating downwards
Pain in upper right arm radiating towards the finger tips dragging in nature
Both of which were relieved on medication and rest
Chest pain with burning sensation since 10 days
Shortness of breath Grade 2 -3
Not relieved on rest
Not associated with vomiting or headaches.
PAST HISTORY
10 days back had an episode of fever which subsided on medication
Not a known case of
Diabetes
Hypertension
Tb
Asthama
Epilepsy
Cvd
FAMILY HISTORY
Not significant
PERSONAL HISTORY
Diet - mixed
Appetite - Decreased
Bowel and bladder - adequate
Allergies -no
Addiction
18 ciggarettes per day and daily intake of alcohol.
GENERAL EXAMINATION
Thin built and malnourished
Vitals
Temperature : Afebrile
Pulse: 81
BP:110/80 mm/ hg
RR :18
SPO2 : 97%
Pallor : present
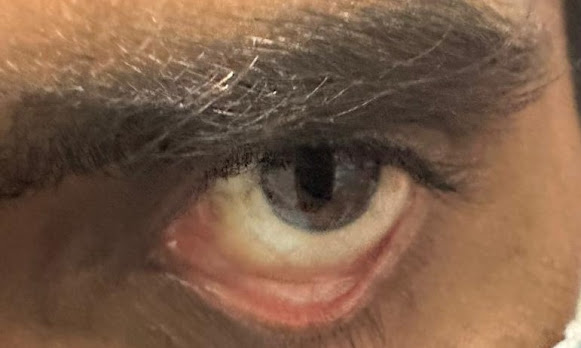
Icterus present
Clubbing absent
Cyanosis absent
Lymphadenopathy absent
Pedal edema absent
JVP RAISED
SYSTEMIC EXAMINATION
CVS
Apex beat 6 th intercoastal space
No thrills
S1 S2 heard
No murmurs
RESPIRATORY SYSTEM
No dyspnoea wheeze
Central trachea
Bilateral air entry +
Bilateral basal crepts +
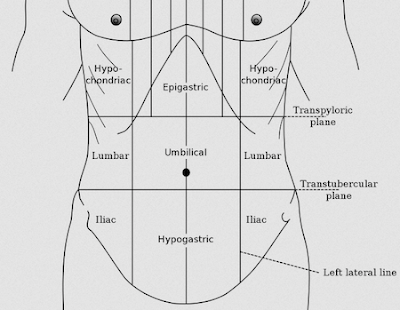
ABDOMEN
Soft
Non tender
CNS
Higher functions
Patient is conscious, coherent,and co operative
Patient is oriented to place not to time and person
Delay in response but able to recall
Cranial nerve intact
Examination of motor system
Tone increased on right upper limb
Not able to approximate both upper limbs
Power of muscle normal
Coordination of movement
Tremors : resting
pill rolling movement
Reflex
Sensory system
Normal
INVESTIGATIONS
Day 1
Day 3
Day 4
Day 5
Day 6
Day 7
Day 8
Day 9
Peripheral blood smear
Peripheral blood smear - 2
PROVISIONAL DIAGNOSIS
BICYTOPENIA
COMMUNITY ACQUIRED PNEUMONIA WITH (BILATERAL LOWER LOBE CONSOLIDATION)
WITH
MODERATE HEPATOSPLEENOMEGALY
WITH
HYPONATREMIA (RECOVERED )2 TO SIADH?
ALTERED MENTATION
Day 1
S :-
Patient is having resting tremors
Delayed speech
Altered sensorium
O:-
Pt is conscious, coherent cooperative
Bp:-140/70
Pr:-92 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-
BICYTOPENIA UNDER EVALUATION
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH PARKINSON'S WITH
MODERATE SPLEENOMEGALY
P:-
Inj AUGMENTIN 1.2g/IV/BD
TAB AZITHROMICIN 500 mg/PO/OD
INJ OPTINEURON 1 amp 100 ml /NS
Vital monitoring
Temperature monitoring
Day 2
S :-
Patient is having resting tremors
Delayed speech
O:-
Pt is conscious, coherent cooperative
Bp:-120/70
Pr:-93 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A
BICYTOPENIA UNDER EVALUATION
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH PARKINSON'S(?)WITH
MODERATE SPLEENOMEGALY
P:-
Inj AUGMENTIN 1.2g/IV/BD
TAB AZITHROMICIN 500 mg/PO/OD
INJ M6RVIG6M1000 micrograms//IV/OD IN 50 ML NS
INJ OPTINEURON 1 amp 200 ml /NS
Vital monitoring
Temperature monitoring
Day 3
S :-
Patient is having resting tremors
Delayed speech
O:-
Pt is conscious, coherent cooperative
Bp:-110/80
Pr:-86 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-BICYTOPENIA UNDER EVALUATION
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH PARKINSON'S(?)WITH
MODERATE SPLEENOMEGALY
P:-
Inj AUGMENTIN 1.2g/IV/BD
TAB AZITHROMICIN 500 mg/PO/OD
INJ M6RVIG6M1000 micrograms//IV/OD IN 50 ML NS
TAB PANTOPRAZOLE 40 MG/PO/OD
Vital monitoring
Temperature monitoring
Day 4
S :-
Patient is having resting tremors
Delayed speech
O:-
Pt is conscious, coherent cooperative
Bp:-110/80
Pr:-86 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-BICYTOPENIA UNDER EVALUATION
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH PARKINSON'S(?)WITH
MODERATE SPLEENOMEGALY
P:-
Inj AUGMENTIN 1.2g/IV/BD
TAB AZITHROMICIN 500 mg/PO/OD
INJ M6RVIG6M1000 micrograms//IV/OD IN 50 ML NS
TAB PANTOPRAZOLE 40 MG/PO/OD
Vital monitoring
Temperature monitoring
Day 5
S :-
Patient is having resting tremors
Fever spikes
Shortness of breath
Pain at bone marrow biopsy site
Delayed speech
O:-
Pt is conscious, coherent cooperative
Bp:-110/70
Pr:-92 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-BICYTOPENIA UNDER EVALUATION(2 to malignancy infection)
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH ESSENTIAL TREMORS WITH
MODERATE SPLEENOMEGALY
P:-
TAB AZITHROMICIN 500 mg /PO/OD
TAB ULTRACET1/2tab /QID
TAB PANTOPRAZOLE 40 MG/PO/OD
INJ PIPTAS 4.5gm /IV/TID
TAB ZINCOVIT OD/PO
Vital monitoring
Temperature monitoring
Day 6
S :-
Patient is having resting tremors
Pain at bone marrow biopsy site
Delayed speech
O:-
Pt is conscious, coherent cooperative
Bp:-120/80
Pr:-98 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-BICYTOPENIA UNDER EVALUATION(2 to malignancy infection)
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH ESSENTIAL TREMORS WITH
MODERATE HEPATOSPLEENOMEGALY
P:-
TAB DOLO 650 mg /PO/OD
TAB ULTRACET1/2tab /QID
TAB PANTOPRAZOLE 40 MG/PO/OD
INJ PIPTAS 4.5gm /IV/TID
TAB ZINCOVIT OD/PO
Vital monitoring
Day 7
S :-
Patient is having resting tremors
Altered behavior GCS E4V4M4
Involuntary Micturation
Fever spikes
Pain at bone marrow biopsy site
Delayed speech
O:-
Pt is conscious
Bp:-110/60
Pr:-130 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
A:-BICYTOPENIA UNDER EVALUATION(2 to malignancy infection)
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH ESSENTIAL TREMORS WITH
MODERATE HEPATOSPLEENOMEGALY
P:-
Riley's tube
Foleys catheter
IVF 3% Nacl at 10ml/hr
INJ MEROPENUM 1g IV STAT
INJ MEROPENUM 1g IV/BD
Temperature charting
Vital monitoring
Ryles feed
Day 8
S :-
Patient is having resting tremors
Altered behavior
Fever spikes
Delayed speech
O:-
Pt is conscious
Bp:-130/70
Pr:-110 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
Kerning sign positive
A:-BICYTOPENIA UNDER EVALUATION(2 to malignancy? infection? )
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH ESSENTIAL TREMORS WITH
MODERATE SPLEENOMEGALY
ACUTE SYMPTOMATIC HYPONATREMIA 2 TO SIADH?
ALTERED SENSORIUM 2 TO HYPONATREMIA? MENINGITIS?
P:-
Riley's tube
Foleys catheter
IVF 3% Nacl at 10ml/hr
INJ MEROPENUM 500 mg IV/BD
INJ OPTINEURON 1 AMP IN 100 ml NS/IV/OD
INJ NEOMOL 1 gm IV/SOS
TAB DOLO
Temperature charting
Vital monitoring
Ryles feed
Day 9
S :-
Patient is having resting tremors
Altered behavior
Fever spikes
Delayed speech
O:-
Pt is conscious
Bp:-110/60
Pr:-120 bpm
Cvs:-s1s2+
R/s:-BLAE +
P/A:- soft , non tender spleenomegaly
CNS:- NAD
Kerning sign positive
A:-BICYTOPENIA UNDER EVALUATION(2 to malignancy? infection? )
WITH
COMMUNITY ACQUIRED PNEUMONIA WITH ESSENTIAL TREMORS WITH
MODERATE SPLEENOMEGALY
ACUTE SYMPTOMATIC HYPONATREMIA 2 TO SIADH?
ALTERED SENSORIUM 2 TO HYPONATREMIA? MENINGITIS?
P:-
Riley's tube
Foleys catheter
IVF 3% Nacl at 10ml/hr
INJ MEROPENUM 500 mg IV/BD
INJ OPTINEURON 1 AMP IN 100 ml NS/IV/OD
INJ NEOMOL 1 gm IV/SOS
TAB DOLO
Temperature charting
Vital monitoring
Ryles feed


























































Comments
Post a Comment