Case of a 46 year male with Type 2 Diabetes Mellitus
This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis "to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
A 46 years old male patient came to the hospital with the chief complaints of :
CHIEF COMPLAINTS
The patient presented to the hospital with the chief complaints of
- Chest pain from 12 years.
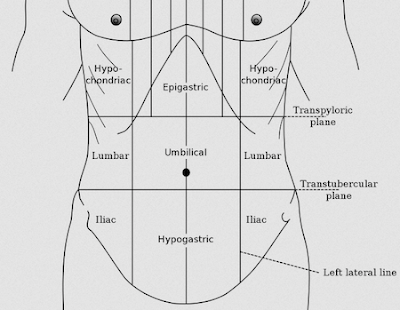
- Generalised abdominal pain predominantly in the right and left flank regions and the lower abdomen from 12 years.
- Pain in the fingers from 12 years.
- Acidity from 10 years.
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 12 years ago, 12 years ago he started experiencing chest pain, abdominal pain predominantly in the right and left flanks and the lower abdomen, and pain in the interphalangeal joints of the fingers. The pain was gradual in onset and increased progressively over the years. The pain was pricking in character and intermittent in nature with one episode of pain every hour. The pain was relieved by taking medication. The pain was not associated with fever, nausea or vomiting.
The patient has been experiencing epigastric pain for the past 10 years, for which he takes pantoprazole 40mg every day. Pain is relieved by taking the medication.
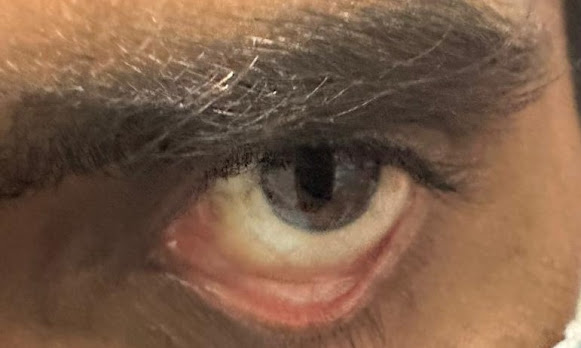
One year ago the patient started experiencing polyuria and polydipsia. On visiting the hospital he was diagnosed with type 2 diabetes mellitus. The patient is not taking any medication and does not have a regulated diet. One year ago the patient also started experiencing blurred vision which causes him headaches on reading.
HISTORY OF PAST ILLNESS
The patient had a bout of pneumonia when he was a child, which caused him chest pain. He recovered after receiving treatment and the chest pain stopped.
He is a known case of Type 2 Diabetes mellitus from 1 year.
He is not a known case of hypertension, asthma, TB, Thyroid condition, CVD, or Epilepsy.
No history of blood transfusions.
FAMILY HISTORY
His father is a known case of Type 2 Diabetes mellitus.
PERSONAL HISTORY
DIET- Mixed diet
APPETITE- Decreased
SLEEP- Adequate
BOWEL AND BLADDER MOVEMENTS - Normal
ADDICTIONS-
ALCOHOL- From 5 years, consumes 1 glass a day.
SMOKING- Chronic smoker- 2-5 cigarettes /day
ALLERGIES- chicken and eggs cause dermatitis.
EXAMINATION
VITALS
BP- 100/80mmHg
PR- 70bpm
AFBRILE
GENERAL EXAMINATION
The patient is conscious, coherent and cooperative.
He is well built and well nourished.
Pallor- Absent
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Koilonychia- Absent
Pedal oedema- Absent
SYSTEMIC EXAMINATION
INVESTIGATIONS
POST LUNCH BLOOD SUGAR
BLOOD UREA
COMPLETE URINE EXAMINATION
HEMOGRAM
LIVER FUNCTION TEST
SERUM CREATININE
SERUM ELECTROLYTES
ECG
FASTING BLOOD SUGAR
USG
GLYCATED HEMOGLOBIN
6 MIN WALK TEST
XRAY
PA VIEW CHEST XRAY
PA VIEW ABDOMEN
MANAGEMENT
1. TAB. Glimepiride 1mg PO/OD
2. TAB. Metformin 500mg PO/OD
3. GRBS Monitoring



.jpg)
.jpg)













Comments
Post a Comment