66 Year old male patient with fever since 10 days.
This is an E log book to discuss our patients de-identified health data shared after
Here we discuss our individual patient problems through series of inputs from available
This E-book also reflects my patients centered online learning portfolio and your
I have been given this case to solve in an attempt to understand the topic of
Chief complaints:
- Fever associated with chills and rigors since 10 days
- shortness of breath at rest
- Pain in the right flank.
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 2 months ago, then he developed fever
Further, he also complained of pain in the right upper quadrant of abdomen,
Patient wakes up at 5 A.M, and smokes numerous beedis, ashe feels that he cannot defecate until he does.
He then heads to work, where he smokes more beedis.
At 6:30 A.M. he gets off from work and then proceeds to completeall his morning ablutions like brushing teeth, going to the restroom,followed by breakfast, a cup of tea and further smoking a full packet of beedis.
He then returns to work, which he briefly resumes for half an hour,owing to lunch break from 2pm to 2:30 pm.
At 5 pm, he is finished with work for the day and rests for an hour, from 6pm to 7pm.After waking up at 7pm, he continues to consume 90mL of alcohol (whiskey) ,along with dinner upon his discretion, depending on whether he is feeling up to itor not on that particular day, especially considering the fact thathe kept experiencing fever every time he ate at night time. The patient notablyexpressed that this was the reason he stopped having dinner since 2 months
. Diet: mixed, 2 idlies/ 2 purses for breakfast along with chutney,
2 cups of rice, along with tomato dal, and vegetable curry along with curd.
Dinner 2 chapatis and tomato dal.
GENERAL EXAMINATION
Vitals
CVS: S1; S2 +,No murmurs heard
RS: BAE +
Crepitations heard in infra axillary, axillary, subscapular regions.
Ronchi are heard in infraclavicular area and axillary area.
CNS: No focal neurological defect
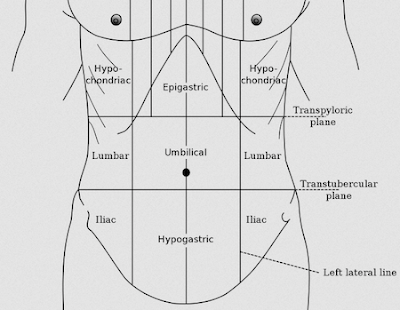
Per Abdomen :
INSPECTION: Shape of abdomen: scaphoid
Umbilicus : inverted
Guarding of abdomen present.
No visible swellings, scars, sinuses ,engorged veins.
Patch present over the right lumbar region
No visible peristalsis or pulsations
PALPATION:
No local rise of temperature
Tenderness present in epigastric region
Liver is palpable, lower border is felt.
On percussion, Liver Span: 13cm
Spleen not palpable, no spleenomegaly.
Percussion: bowel resonance felt.
On auscultation, normal bowel sounds are heard.
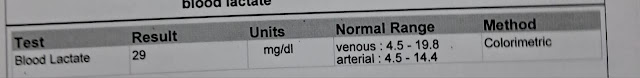
INVESTIGATIONS
HEMOGRAM

.jpeg)



.jpeg)

.jpeg)
.jpeg)
.jpeg)

.jpeg)

Comments
Post a Comment